January 30, 2026
January 30, 2026
Cervical cancer: Sierra Leone’s silent killer of women
For months, Ramatulai Kamara endured pain during the most intimate time in her marital life.
“When I had sexual intercourse with my husband, I bled. I felt pain,” she recalls, recounting her experience with cervical cancer, a type of cancer that affects the cervix, which is causing havoc among women in Sierra Leone and across the world.
Most cases of this preventable disease are caused by an infection with the Human Papillomavirus (HPV), which is mostly gotten through sexual contact and usually develops slowly over time.
Cervical cancer is the fourth most common cancer among women globally. The most recent available data from the World Health Organization (WHO) shows that there were 662,301 new cases in 2022. In that same year there were roughly half as many deaths from cervical cancer worldwide. Low-income countries, including Sierra Leone, bear the burden of the disease, estimated at around 85 percent.
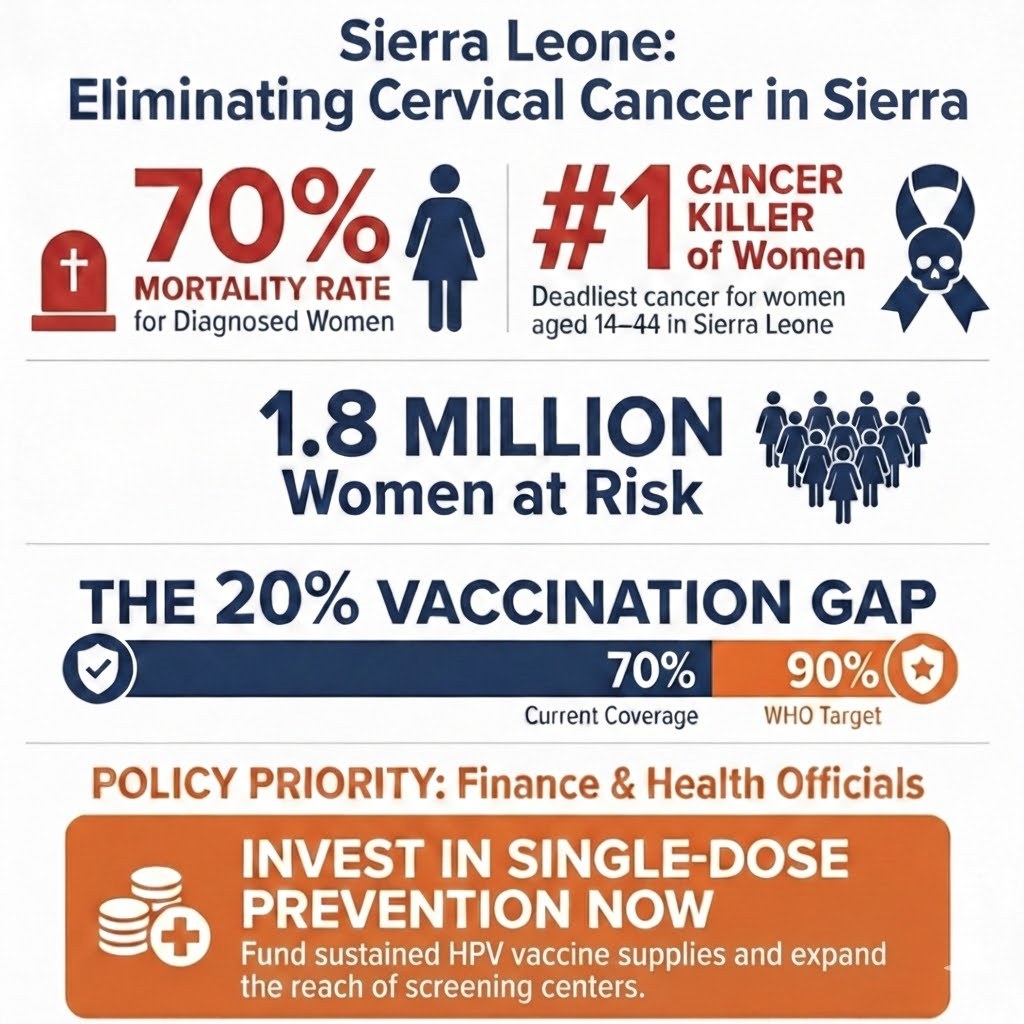
Data from the National Cancer Registry in the Ministry of Health (MoH) reveals that cervical cancer is the second most common cancer in Sierra Leone, after breast cancer, and the number one killer of all cancers among women aged 14 to 44 years. The data also show an estimated 500 new cases of the disease are diagnosed every year, with over 70 percent of those diagnosed dying from it. But some observers believe that these figures are highly underestimated, due to a lack of awareness and consequently low testing rates.
“The death rate for cervical cancer among women in Sierra Leone is high mainly because most victims are diagnosed late,” says Amanda Clemens, Social Mobilization Coordinator at the Expanded Programme on Immunization in the Health Ministry. She notes that early detection and treatment are crucial for survival.
But as the story of Ramatulai reveals, the situation for Sierra Leoneans is made dire due to limited available diagnostics and treatment options in-country. After months of going through pain in silence for lack of knowledge, she visited a nearby hospital in her community, where nurses prescribed treatment based on symptoms she described. The bleeding did stop. But it resumed one year later. This time, she also endured the pain for a long time without telling anyone, and she didn't seek medical treatment. It got worse with time, and eventually she returned to the hospital. This time around, she was tested. When the result came back, Ramatulai was referred to Sierra Leone’s main referral hospital, Connaught, with no explanation. There, nurses only read her results and referred her to a doctor, who broke the sad news to her.
“I felt bad. I cried,” she recalls her reaction on learning that she had been dealing with cervical cancer. But luckily for Ramatulai, it was Stage one cervical cancer. This means the disease had not spread beyond the cervix. But she needed surgery, and she was told that it was available only in Ghana at the time, requiring thousands of US dollars. That was impossible for a mere petty trader like her.
For the earliest stages of cervical cancer, either surgery or radiation combined with chemotherapy may be used as treatment. For advanced stages, radiation combined with chemotherapy is usually the primary treatment. Either of these is extremely expensive for the average Sierra Leonean. Ramatulai says she was placed on some chemotherapy, which was very expensive for her and her family. Eventually, an “opportunity” came for surgery locally.
In the last four years, Sierra Leone has prioritized a response to cervical cancer, focusing on preventive measures: Vaccination is one of its key strategies towards elimination, as well as screening. The vaccine provides protection for women and girls against HPV and the risk of cervical cancer.
The government, with the help of partners, notably the Global Vaccine Alliance (Gavi) and the United Nations, introduced the HPV vaccine into the country’s routine immunization programme in 2022. The programme generally targets girls outside the sexual age, while those with sexual experience are screened for early detection and timely treatment. According to the Health Ministry, more than 1.8 million women of reproductive age in the country are at risk of HPV.
In 2023, the national effort against HPV intensified when the government and its partners launched a National Cervical Cancer Elimination Strategy. This is in line with WHO's global strategy to eliminate the disease by 2030, through accelerating the attainment of key milestones: vaccine coverage by 90%, screening of 70% of women of reproductive age (by age 35), and providing timely treatment to 90% of those diagnosed with the disease. Current vaccination coverage in Sierra Leone is 70%, leaving a 20-percentage-point gap to reach the WHO target.
The routine immunization programme is targeted at girls aged 10 to 14. And this year, for the third time, the government has also embarked on a mass immunization campaign. Clemence says this is in line with WHO’s recommendation that children 9 to 14 years are prioritized for vaccination, while those above are screened and treated.
“One of the reasons why we vaccinate children at that age is that they haven’t yet started sexual activity. For people who have started sexual activity, which is above that age, we are advised for them to do screening,” she explains.
“HPV is transmitted through sex, and for children at 10 years, we assume they haven’t got their sexual debut, so they will have the protection needed. The campaign is to cover a lot more children. Vaccines are not curative; they are preventive. So, with the campaigns, we intend to prevent as many more girls as possible within the age range.”
In 2022, when the HPV vaccine was introduced for the first time, a campaign was also launched targeting 153,991 girls with the vaccine, each receiving two doses over a six-month period. Between the two campaigns, over 500,000 girls received the vaccine, according to the government. The goal, says Dr. Jalikatu Mustapha, Deputy Minister of Health II, is to eradicate cervical cancer in the country within the next two decades.
“What makes cervical cancer particularly tragic is that it is one of the few cancers that can actually be prevented through a simple and effective vaccine,” she says at a government press briefing held on the eve of the latest campaign.
“No woman in Sierra Leone should ever die again from a disease that can be prevented,” she stresses.
This latest campaign, conducted from November 17t-23, 2025, targeted one million girls between the age 11 and 18. And it is also the first time since Sierra Leone switched from two doses to a single dose of the HPV vaccine. It also coincided with the first-ever global commemoration of World Cervical Cancer Elimination Day set during the 78th World Health Assembly in 2025.
The HPV vaccine, certified safe and effective by WHO, has been available in most developed countries since the 2000s. Sierra Leone became the 19th country in Africa to introduce it back in 2022.
Gavi not only supported the procurement of the vaccines, it also funded procurement and installation of hundreds of solar refrigerators to help strengthen cold chain systems.
Alongside vaccination, the government and its partners say they established 24 cervical cancer screening and treatment centers across all districts—including seven in the western area of Sierre Leone. Each site is equipped with trained health workers and diagnostic tools that allow women to be screened, diagnosed and treated immediately they are diagnosed.
Community Health Officer Emmanuel Nyoko is one of hundreds of healthcare workers executing this strategy. He is the In-Charge of the Wellington Community Health Center, a heavily populated suburb in the eastern part of Freetown. The center caters for a population of 26, 540 people. Among other strategies, it collaborates with schools to facilitate access to the children.
Prior to the 2022 introduction of the HPV vaccine, the Health Ministry and Gavi in 2014 undertook a pilot vaccine roll out in the southern Bo District. This was when the country’s ability and readiness to implement a school-based vaccination programme nationwide was established.
“We have specific days that we visit the schools and administer the vaccines as part of our regular community outreach,” Emmanuel explains. His team also works with Community Health Workers, a group of local volunteers who help mobilize people in hard-to-reach communities for necessary health interventions, to reach out-of-school children with the HPV vaccine.
Thanks to mis- and disinformation campaigns, there have been genuine expression of fears among parents and guardians, which has led to apathy towards vaccine acceptance generally, making the job of Emmanuel and his team difficult and threatening the country’s chance of meeting its coverage target. The Wellington Community Health Center management sought to overcome this challenge by creating a WhatsApp forum where community members are given the opportunity to express their concerns and are provided answers to their questions.
From January to October of 2025, the Wellington Community Health Center diagnosed only one case of cervical cancer, and Emmanuel believes this is a testament to the fact that the vaccination exercise and awareness raising efforts are paying off. “The coverage is encouraging because the acceptance is high,” he says.
Data provided by the ministry show that over 33,000 women have been reached with screening services in one year since the centers were created across the 16 districts of the country.
But Emmanuel warns that the focus should be to sustain this momentum. And this would require uninterrupted supply of the vaccines as well as provision of the resource to maintain sensitization both on cervical cancer prevention measures and the safety of the vaccines, he notes.
The Health Ministry says some level of training has been provided for local surgeons to perform cervical cancer operations in the country. It also says it has established local hospice care units for women in advanced stages of the disease, providing palliative care and comfort.
“As a ministry, we are deeply passionate about this cause,” says Dr. Mustapha, who disclosed that her own grandmother died of cervical cancer at a time when there was little understanding of the disease locally.
“Today, we have the tools and the knowledge to prevent it—and we will,” she tells reporters.
Written by Global Health Advocacy Incubator Partner Health Alert—Sierra Leone; illustrated by Abel Akara Ticha of the Global Health Advocacy Incubator.